Herz/en: Unterschied zwischen den Versionen
Becher (Diskussion | Beiträge) (Die Seite wurde neu angelegt: „'''Pulmonary valve (valva trunci pulmonalis)'''<br> The pulmonary valve prevents the backflow of blood into the right ventricle. Since this valve is located be…“) |
Becher (Diskussion | Beiträge) |
||
| (26 dazwischenliegende Versionen desselben Benutzers werden nicht angezeigt) | |||
| Zeile 19: | Zeile 19: | ||
<div class="box"> | <div class="box"> | ||
<div class="pic">__TOC__</div> | <div class="pic">__TOC__</div> | ||
| − | <div class="segmenter"><segmenter-embedding wsemb-id="herzteile" file="Herzteile.seg" height="300" width="400"/></div> | + | <div class="segmenter"><segmenter-embedding public wsemb-id="herzteile" file="Herzteile.seg" height="300" width="400"/></div> |
</div> | </div> | ||
| Zeile 188: | Zeile 188: | ||
The pulmonary valve prevents the backflow of blood into the right ventricle. Since this valve is located between two low-pressure systems (venous limb of the systemic circulation and pulmonary circulation), it is thinner. | The pulmonary valve prevents the backflow of blood into the right ventricle. Since this valve is located between two low-pressure systems (venous limb of the systemic circulation and pulmonary circulation), it is thinner. | ||
| − | ''' | + | '''Aortic valve (valva aortae)'''<br> |
| − | + | The aortic valve prevents backflow from the aorta into the left ventricle. It has a slight outward bulge (sinus aortae). The coronary vessels ( a. coronaria sinistra and dextra) originate in the left and right sinus aortae, so that the heart is supplied with blood. | |
| − | == | + | ==Cardiac auscultation== |
| − | + | In the case of a malfunction, audible flow noises are caused by the formation of whirls in the blood. Cardiac auscultation is an old but important method for recognizing these sounds. It is used both for the initial detection and the follow-up of functional disorders. The basis is that two sounds can be heard in a healthy adult heart. The first heart sound (S1) is at the beginning of systole. The tone is produced by the blood column hitting the leaflet valves and not, as is often assumed, by the closure of the valves. The second heart sound (S2) is produced by the closure of the leaflet valves at the end of systole. It is much brighter than the first heart sound. The two sounds are clearly audible at different locations. The first heart sound is clearly heard above the apex of the heart, whereas the second heart sound is clearly heard above the base of the heart. At Erb's point, which is located on the left parasternal side in the third intercostal space, all heart valves can be detected equally well. Specific points on the chest are recommended for auscultation of individual heart valves, as the sounds are projected to these locations and can thus be heard loudest: | |
| − | * | + | * Aortic valve: 2/3rd intercostal space right parasternal. |
| − | * | + | * Pulmonary valve: 2nd intercostal space left parasternal |
| − | * | + | * Tricuspid valve: 4th intercostal space right parasternal |
| − | * | + | * Bicuspid valve: 5th intercostal space left medioclavicular |
| − | == | + | ==Excitation formation and excitation conduction system <i>(Coming soon)</i>== |
| − | + | In the heart there is an autonomous excitation generation system (systema conducente cordis) and an excitation conduction system (systema conducente cordis). A distinction is made between four sections. When the heart is excited, the atrial and ventricular muscles contract about 100,000 times a day. The heart muscle is controlled by electrical impulses. The resulting impulses spread through a special cell system of the heart muscle. | |
| − | === | + | ===Sinus node=== |
| − | + | The sinus node is also called the nodus sinuatrialis or Keith-Flack node. Macroscopically, it consists of a muscular structure that is about 3 mm thick and 10 mm long. The external shape resembles a comma. It is located on the dorsal side of the right heart, subepicardially in the terminal sulcus. Cranial to the sinus node is the junction of the superior vena cava. In some cases, the sinus node extends into the right heart ear. | |
| − | + | Functionally, the sinus node is the primary pacemaker centre of the heart and is therefore involved in the complex regulation of the heart rate. The sinus node has the central role of excitation formation. It generates excitation volleys with a resting frequency of 60-70 impulses per minute. The pulses are used to excite the atrial myocardium, as the atrial excitation wave propagates towards the ventricles. The sinuatrial ramus nodi provides blood flow to the sinus node. It is controlled by the sympathetic and parasympathetic nervous systems. The sinus node consists of specific heart muscle cells: | |
| − | '''P | + | '''P cells'''<br> |
| − | + | The P cells (''pacemakers'') are roundish, pale cells that are usually present in groups. They are connected to each other by nexus and desmosomes. | |
| − | ''' | + | '''Transition cells'''<br> |
| − | + | Transition cells are elongated and partially branched cardiomyocytes. They contain a large number of myofibrils. The transition cells connect the P cells and establish a connection to the working myocardium. | |
| − | === | + | ===Atrioventricular node=== |
| − | + | The atrioventricular node is also called the nodus atrioventricularis, AV node or Aschoff-Tawara node. It is the secondary pacemaker centre of the heart. The AV node is 5 mm long, 3 mm wide and 1 mm thick and is located in the right atrium. Its exact location is at the base of the atrial septum before the confluence of the coronary sinus. This area is called the triangle of Koch. The atrioventricular node serves to regulate stimulus exaggeration via the non-conducting cardiac skeleton. It is continued by the His bundle, which continues towards the apex of the heart. The AV node is also controlled by the sympathetic and parasympathetic nervous systems. Blood flow takes place through the ramus nodi atrioventricularis from the arteria coronaria dextra. Its main function is to delay the transmission of excitation to the ventricles. This ensures that the atrial contraction is completed before the ventricular contraction begins. Spontaneous excitations can also be generated by the AV node. However, these have a much lower frequency (40-50 depolarisations per minute) than the sinus node. This impulse excitation does not take place as long as the sinus node is intact. | |
| − | === | + | ===Atrioventricular bundle=== |
| − | + | The atrioventricular bundle, also known as the fasciculus atrioventricularis, AV bundle or His bundle, is a component of the heart's conduction system. It is 4 mm thick and 20 mm long. The AV bundle originates subendocardially in the atrium from the AV node. It penetrates the trigonum fibrosum dextrum and then divides into the two tawara legs in the pars membranacea of the ventricular septum. The function of the AV bundle is to transmit excitation from the AV node to the ventricular legs. | |
| − | === | + | ===Bundle branch=== |
| − | + | The bundle branches are also called crus dextrum and sinistrum or tawara branches. The tawara legs divide at the AV bundle. Their main function is to transmit excitation from the His bundle via the nexus into the working myocardium. The left Tawara branch (crus sinistrum) branches off almost perpendicularly from the His bundle and then fans out. This creates the following structures: posterior fascicle, middle fascicle and anterior fascicle. The right tawara limb (crus dextrum) continues anteriorly and enters the myocardium of the ventricular septum. It continues towards the apex of the heart. In the ventricular myocardium, excitation is transmitted via the Purkinje fibres. | |
| − | == | + | ==Diseases== |
| − | *[[Special:MyLanguage/Herzinfarkt| | + | *[[Special:MyLanguage/Herzinfarkt|Myocardial infarction]] |
| − | *[[Special:MyLanguage/Herzinsuffizienz| | + | *[[Special:MyLanguage/Herzinsuffizienz|Cardiac Failure]] |
| − | *[[Special:MyLanguage/Herzrhythmusstörung| | + | *[[Special:MyLanguage/Herzrhythmusstörung|Cardiac arrhythmia]] |
| − | == | + | ==Free exploration== |
| − | {{Tab4|Button1= | + | {{Tab4|Button1=Heart|Button2=Heart vessels|Button3=Internal spaces in the heart|Button4=Heart in situ|Segmenter1=<segmenter-embedding public wsemb-id="herzteile" file="Herzteile.seg" height="300" width="500"/>|Inhalt1=<b>Structure of the heart</b><br>Look at the heart in 3D and explore it freely. Afterwards, you can look at other cases or check your acquired knowledge through the practice exercises.|Segmenter2=<segmenter-embedding public wsemb-id="Herzgefäße" file="Herzgefaesse.seg" height="300" width="500"/>|Inhalt2=<b>Heart vessels</b><br>Look at the vessels that connect the heart to the body and pulmonary circulation as well as some coronary vessels.|Segmenter3=<segmenter-embedding public wsemb-id="HerzBinnenraeume" file="HerzBinnenraeume.seg" height="300" width="500"/>|Inhalt3=<b>Internal spaces in the heart</b><br>Look at the internal spaces in the individual parts of the heart.|Segmenter4=<segmenter-embedding public wsemb-id="HerzInSitu" file="HerzInSitu.seg" height="300" width="500"/>|Inhalt4=<b>Heart in situ</b><br>Look at the heart in situ.}} |
| Zeile 242: | Zeile 242: | ||
<div class="clear aufgaben" style="margin-bottom:1em;"> | <div class="clear aufgaben" style="margin-bottom:1em;"> | ||
<div class="menu_item"> | <div class="menu_item"> | ||
| − | <div | + | <div><li class="mw-ui-button button_new" >[[Special:MyLanguage/Übungsaufgaben|Exercises]]</li></div> |
</div> | </div> | ||
</div> | </div> | ||
| Zeile 248: | Zeile 248: | ||
<div class="clear aufgaben"> | <div class="clear aufgaben"> | ||
<div class="menu_item"> | <div class="menu_item"> | ||
| − | <li class="button_article | + | <li class="button_article"><b>Further article</b></li> |
</div> | </div> | ||
<div class="menu_item"> | <div class="menu_item"> | ||
| − | <li class="mw-ui-button button_normal">[[Special:MyLanguage/Niere (Ren)| | + | <li class="mw-ui-button button_normal">[[Special:MyLanguage/Niere (Ren)|Kidney]]</li> |
</div> | </div> | ||
<div class="menu_item"> | <div class="menu_item"> | ||
| − | <li class="mw-ui-button button_normal">[[Special:MyLanguage/Humerus| | + | <li class="mw-ui-button button_normal">[[Special:MyLanguage/Humerus|Humerus]]</li> |
</div> | </div> | ||
</div> | </div> | ||
| Zeile 263: | Zeile 263: | ||
---- | ---- | ||
| − | [[Category: | + | [[Category:Organ system]] |
</div> | </div> | ||
<languages/> | <languages/> | ||
Aktuelle Version vom 11. Mai 2022, 07:24 Uhr
The heart (lat. cor) is a hollow muscle. Through its contractions the blood is pumped through the body. It is a vital organ that ensures the necessary supply of blood to the other organs.
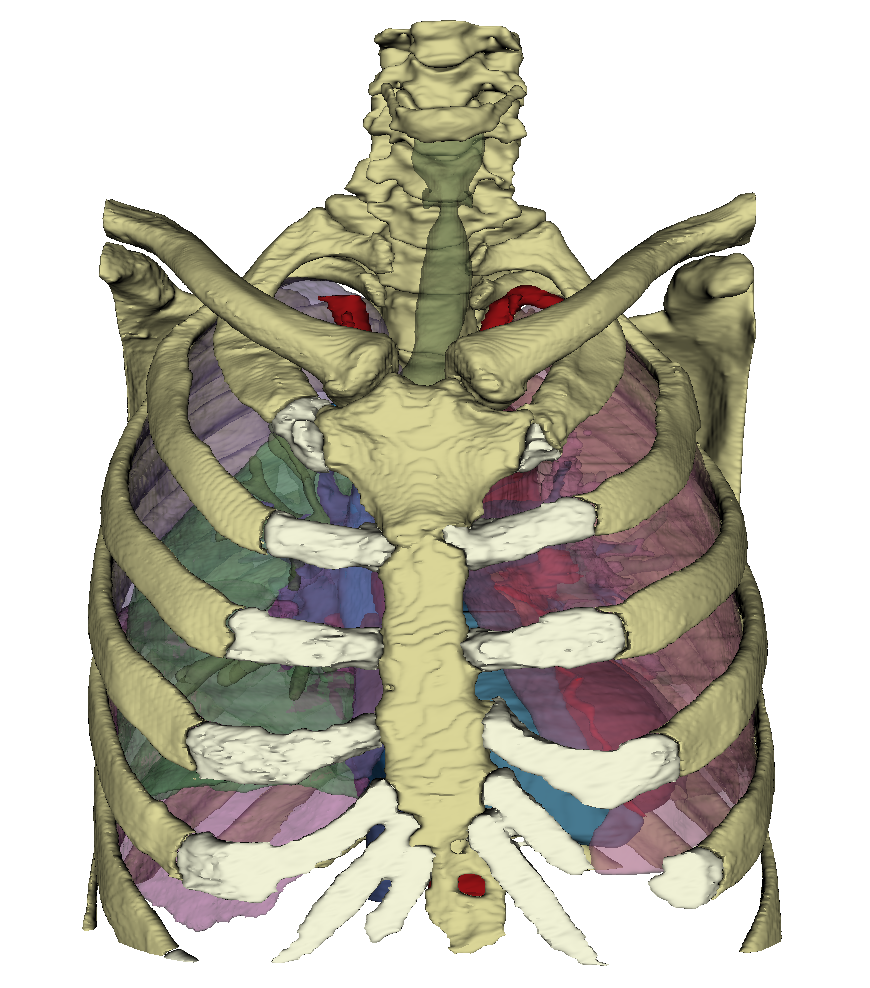
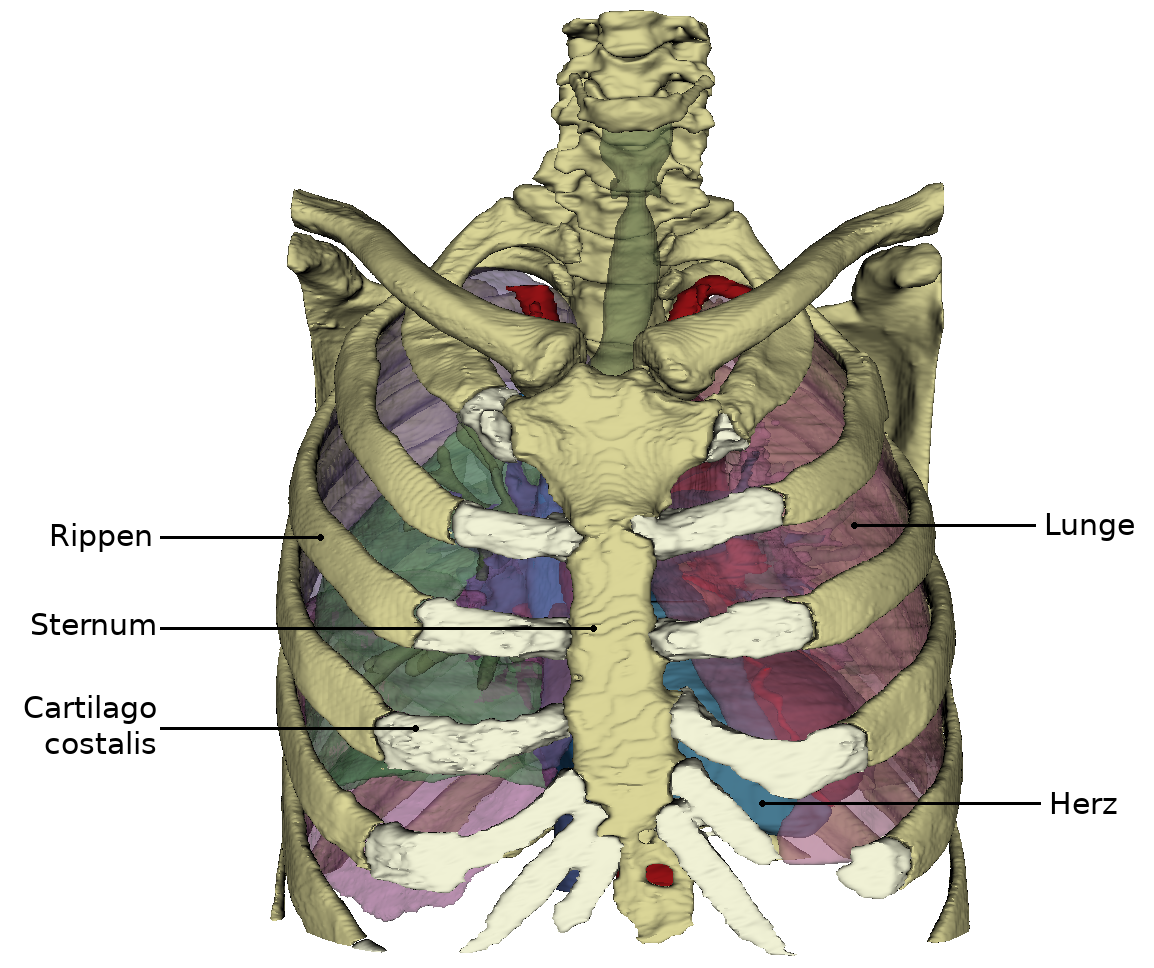
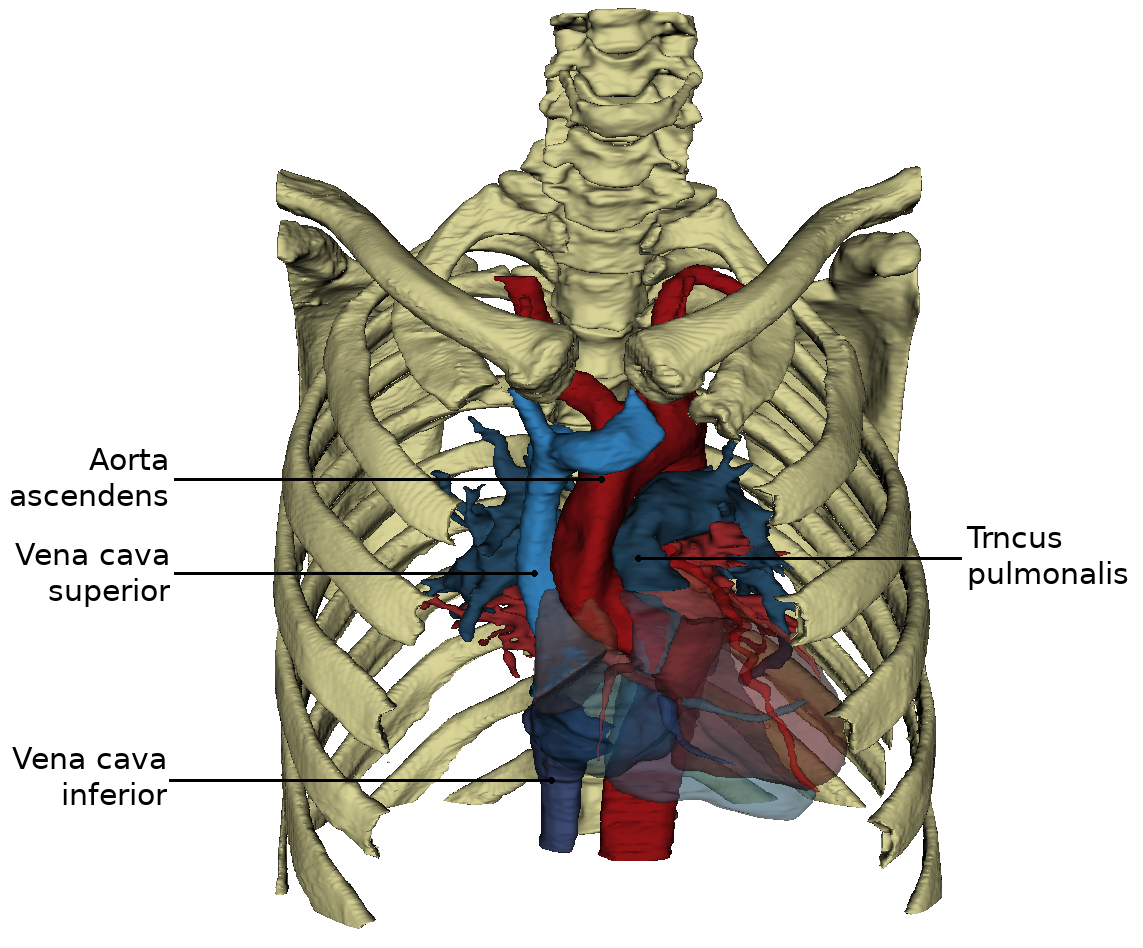
Heart in situ
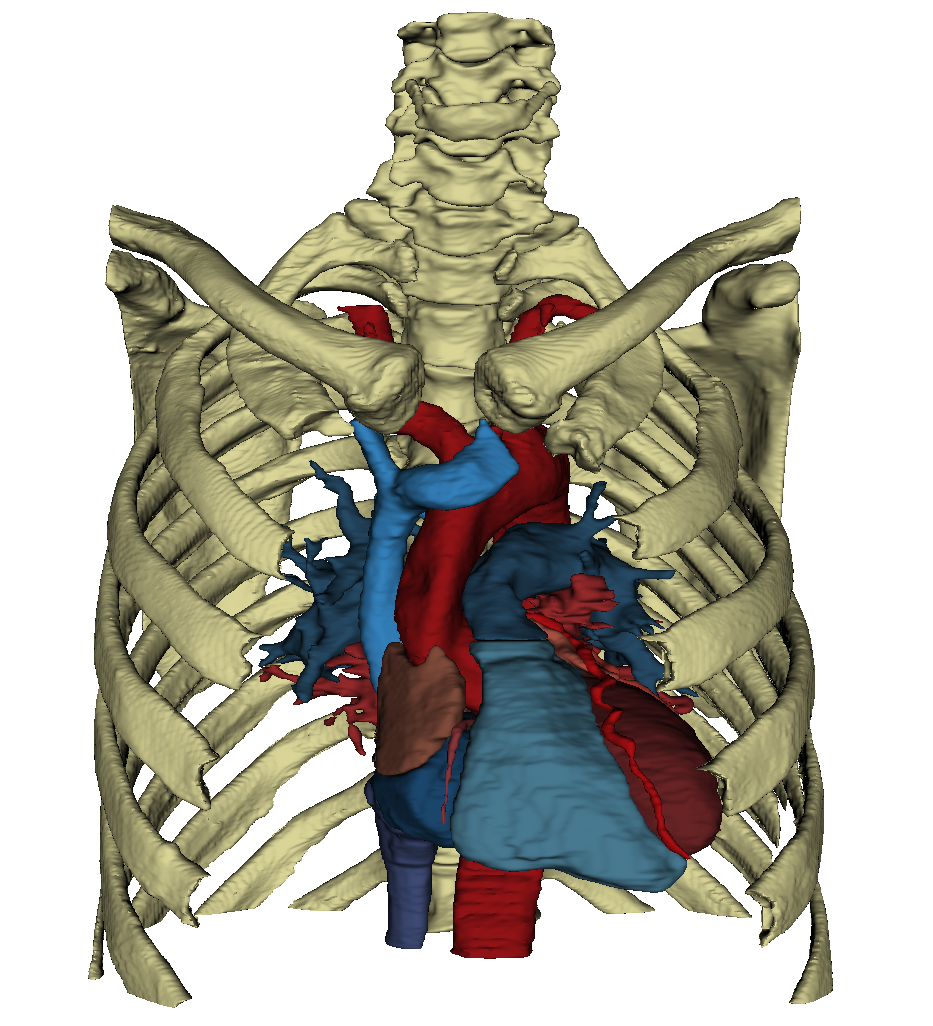
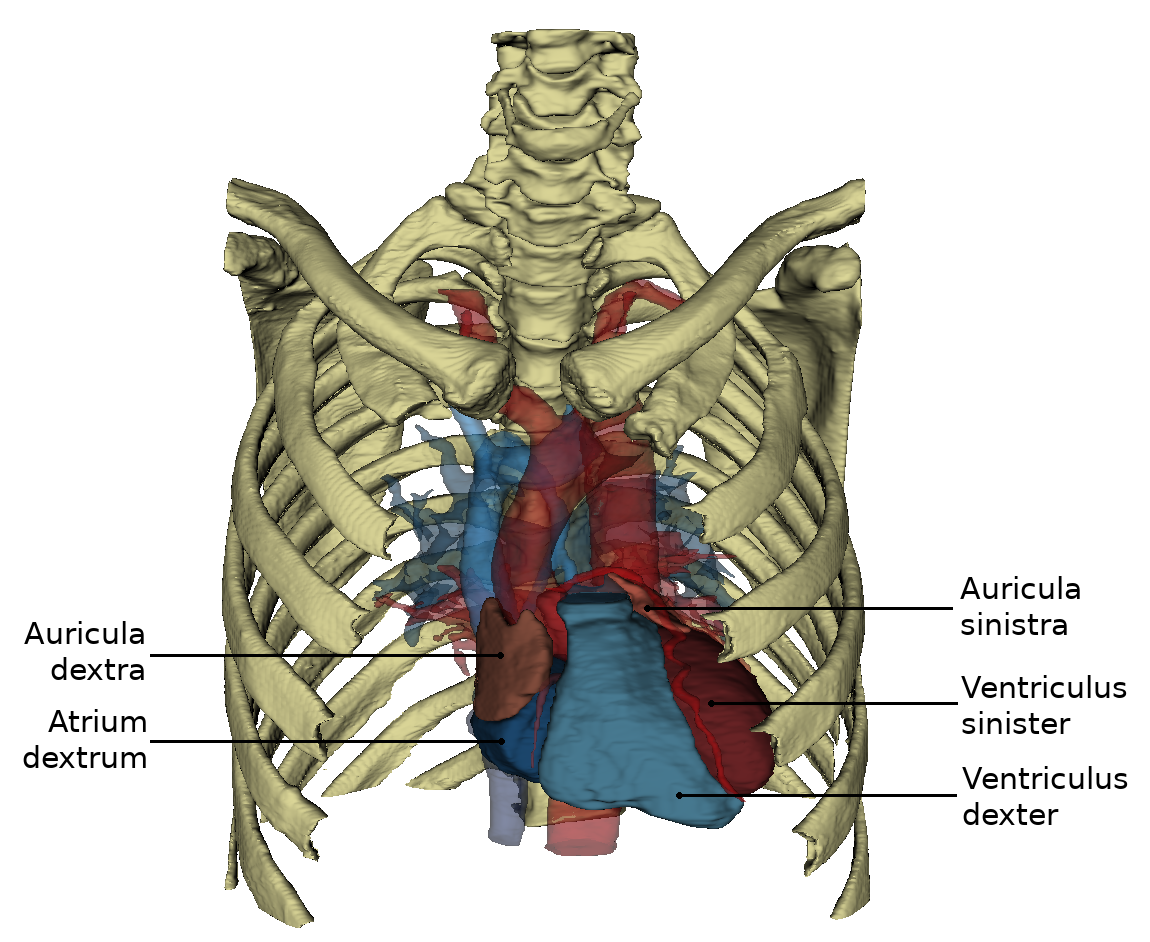
The heart is located approximately in the middle of the thorax, which is called the mediastinum. The representation in the WebViewer is greatly simplified. In order to have a clear view of the heart, the thorax must be opened extensively and the connective tissue in the mediastinum anterius removed. Approximately two-thirds of the heart is located to the left of the breastbone and one-third to the right. The apex of the heart (apex cortis) points to the left front and lies on one level with the left nipple. Its contraction (the so-called cardiac apex thrust) can be felt as a tender beat through the chest wall. Viewed ventrally, the heart is located obliquely and turned counterclockwise in the thorax. At the front it reaches the sternum and at the back it is bounded by the trachea and oesophagus. On the left and right it is surrounded by the lungs. The right ventricle is clearly visible from the ventral view. The left ventricle is only partially visible. Even the large vessels are not all visible at the base of the heart. The vv. pulmonales lies on the flip side of the heart and merges in the left atrium, which is also dorsal. Clearly recognizable, however, are the two heart ears (auricula sinistra and dextra), each located on the periphery.
Form and structure
View from ventral
The heart (Cor) has the shape of an obliquely inclined cone and is a muscular hollow organ.
The following structures are differentiated in the heart:
- a downward, left and ventrally inclined tip of the heart,
- three areas, whose names are mostly based on the adjacent thorax walls
- a heart base inclined upwards, to the right and dorsally
On the side of the heart that rests on the sternum and costae, you can see the right ventricle, which is separated from the left ventricle by the sulcus interventricularis anterior. From this angle, the left ventricle forms the left edge of the heart and the apex cordis.
The anterior interventricular groove (sulcus interventricularis anterior) contains the r. interventricularis anterior of the a. coronaria sinistra and the v. interventricularis anterior. The sulcus interventricularis anterior describes the course of the ventricular septum inside the heart.
The atria (atrium sinistrum and dextrum) are separated from the ventricles by the sulcus coronarius, which also contains coronary vessels.
The right atrium (auricle dextra) attaches to the base of the aorta (pars ascendens), the left atrium (auricle sinistra) to the base of the truncus pulmonalis. From this perspective, the aorta obscures the exit of the right pulmonary artery from the pulmonary trunk.
View from dorsal and caudal
By turning the heart ventrally, the side facing the diaphragm (Fascies diaphragmatica) becomes more visible. Exclusively from caudally from the viewing direction of the diaphragm it can be seen that the both Vv. cavae lie in one axis.
View from dorsal
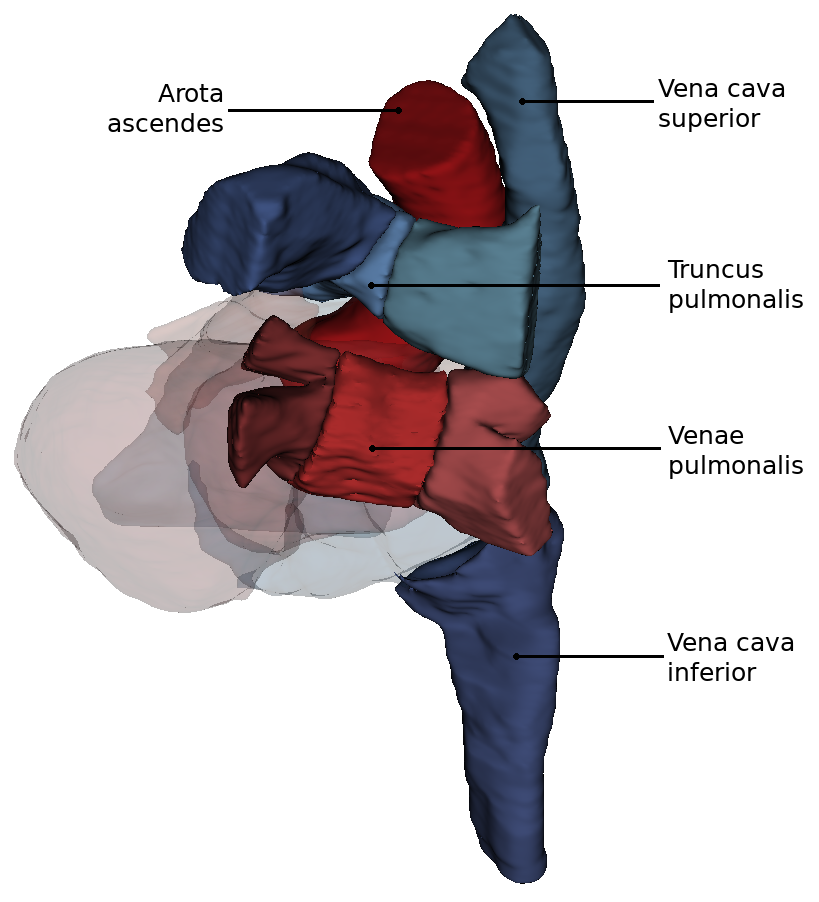
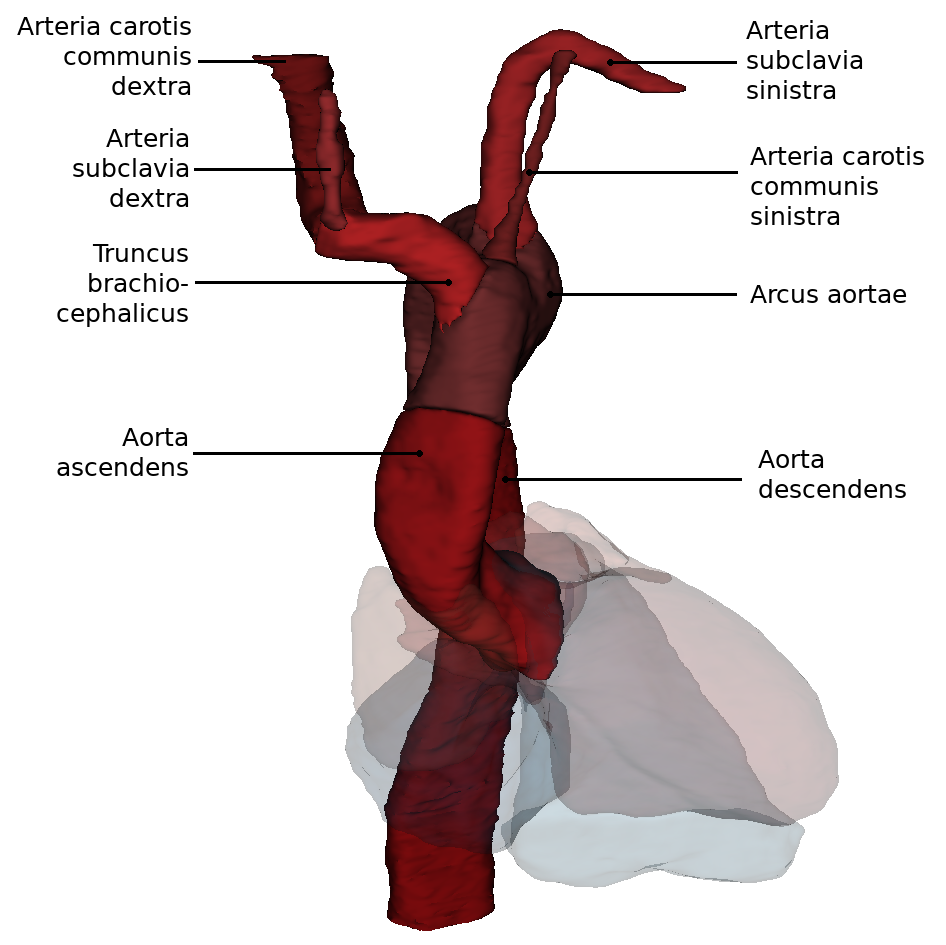
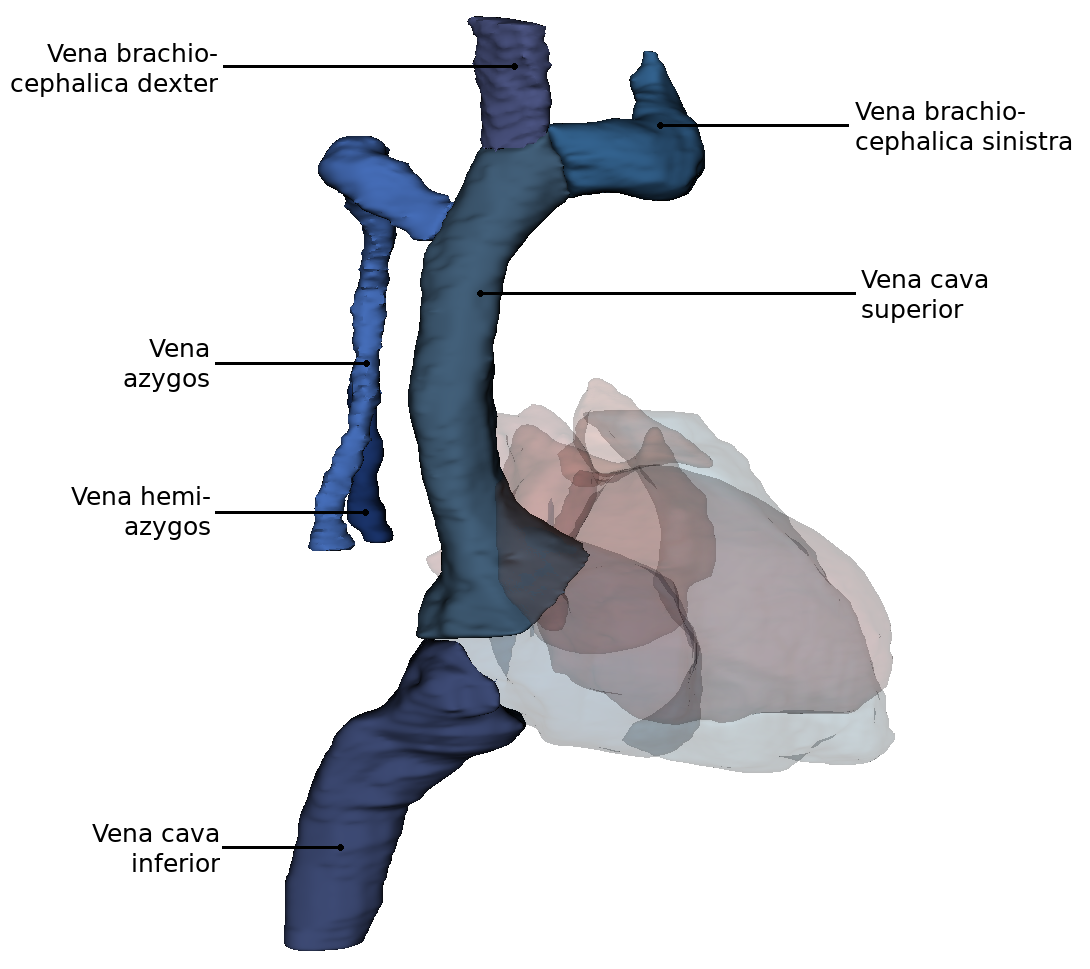
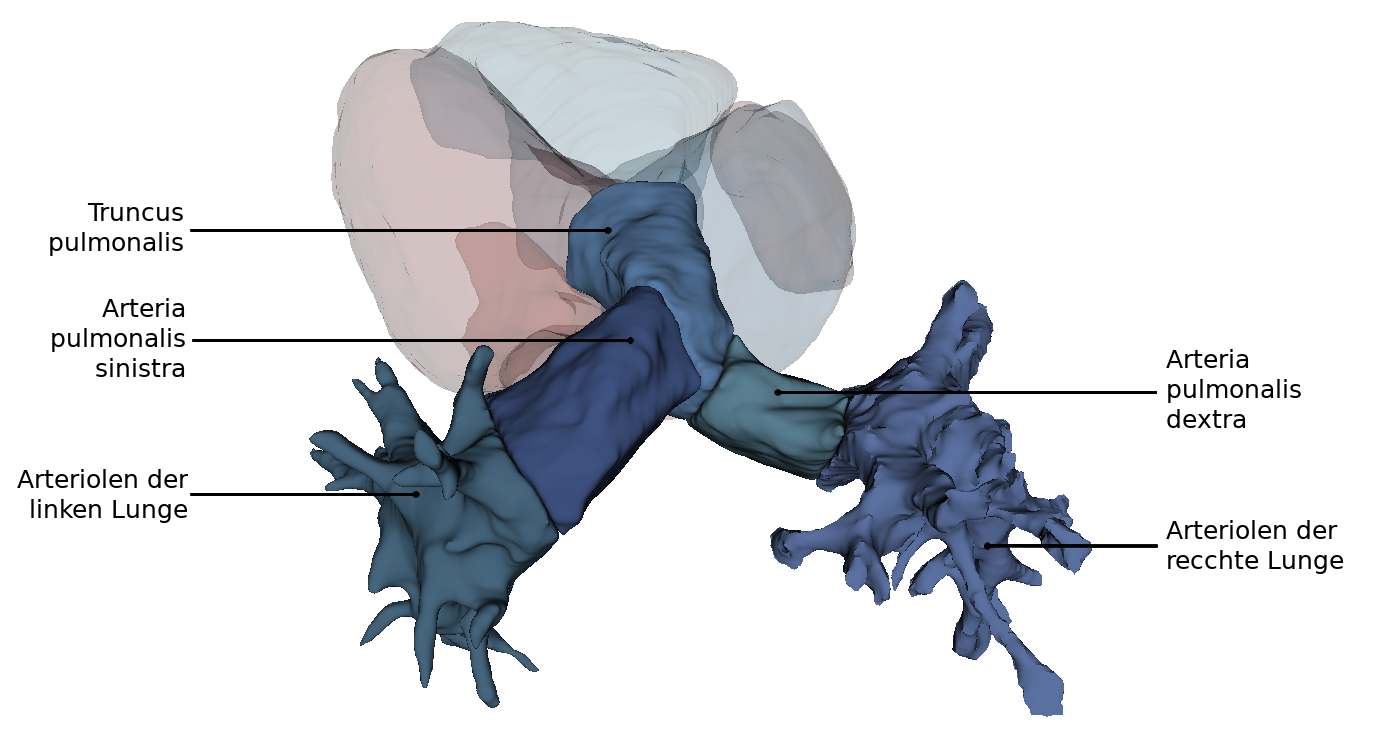
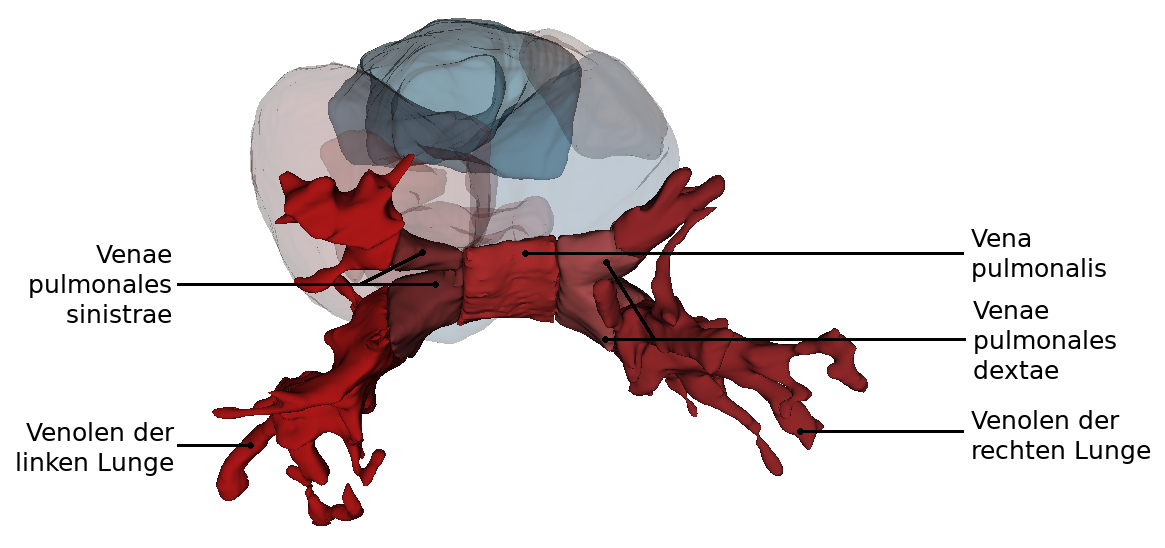
From this perspectiveit is clearly visible how the Arcus aortae crosses the Truncus pulmonalis, where it divides into the A. pulmonalis sinistra and A. pulmonalis dextra. At this point the three major arteries branch off to the upper extremity and to the neck and skull: Truncus brachiocephalicus, A. carotis communis sinisra and A. subclavia sinistra. Also the orifices of the - usually four - Vv. pulmonales into the left atrium (Atrium sinistrum) and the two Vv. cavae into the right atrium (Atrium dextrum) are well visible. Also visible here is the sinus coronarius in the sulcus of the same name. This sinus is the collection vessel for the venous blood that is supplied to the heart via the Vv. cardiacae.
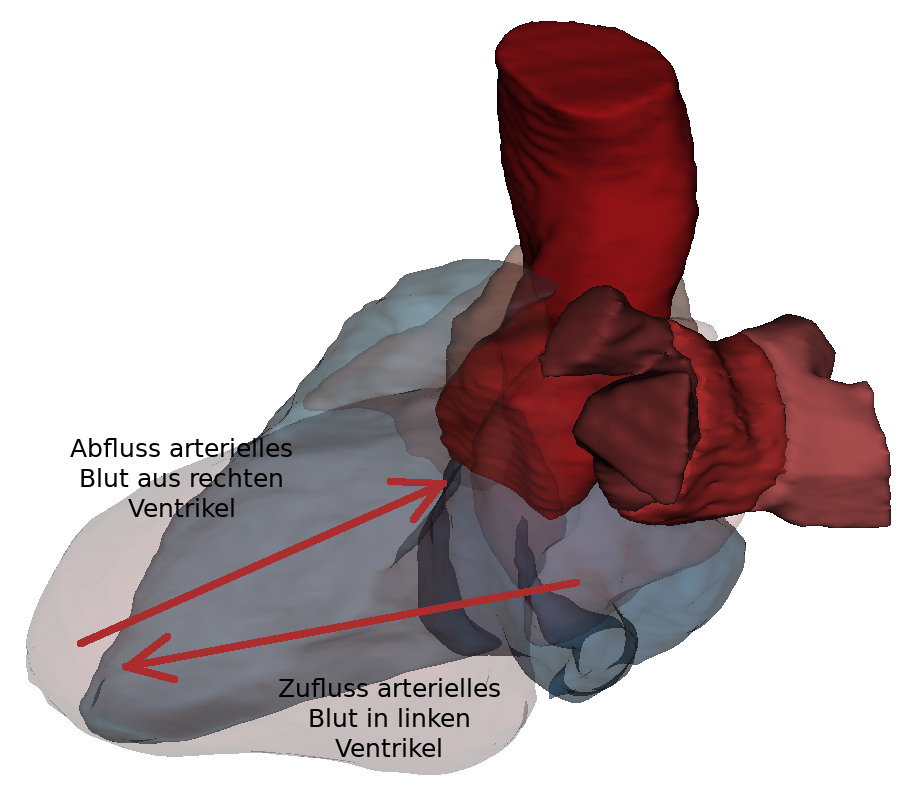
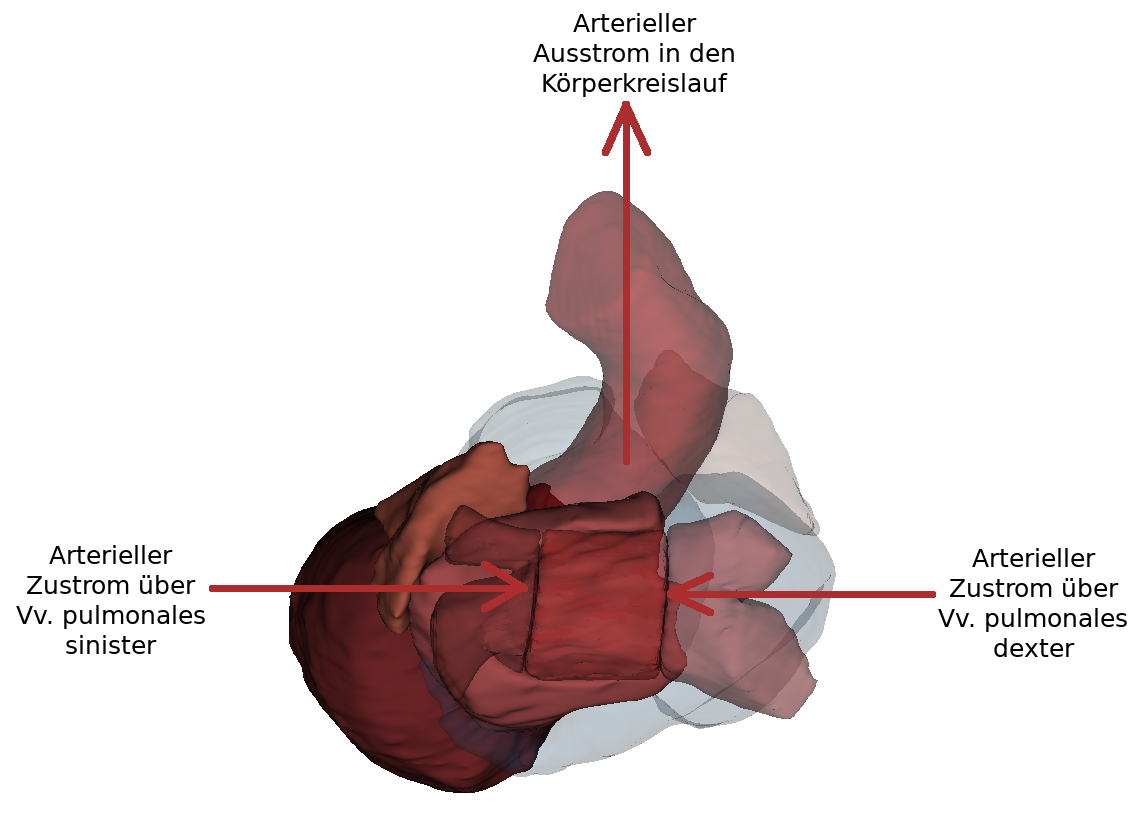
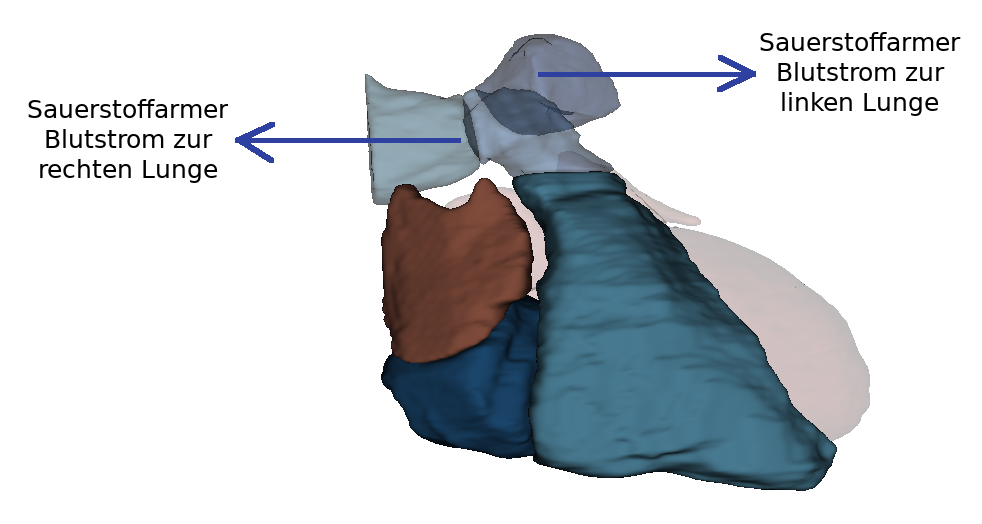
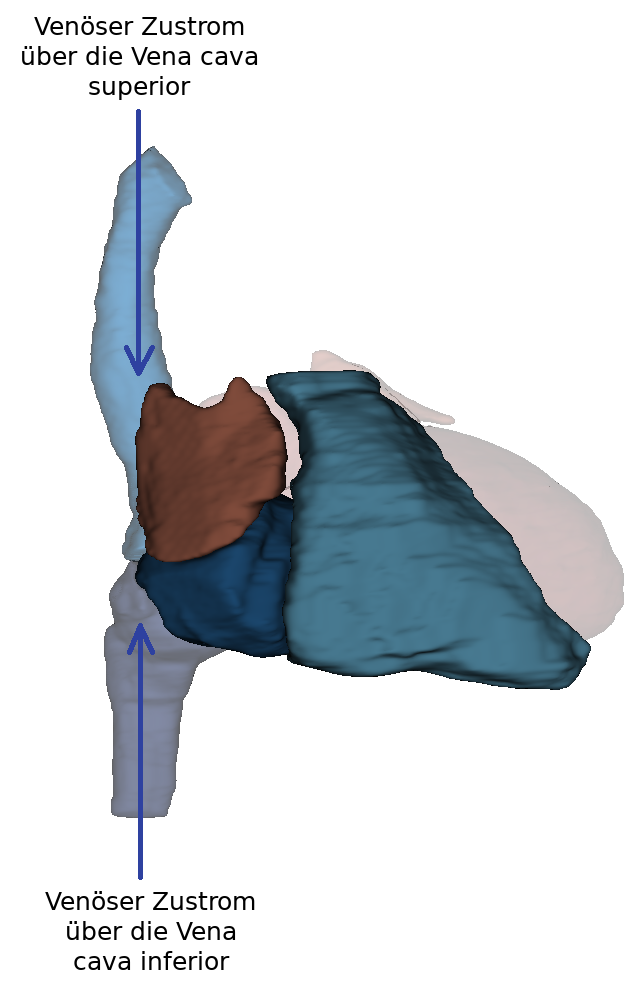
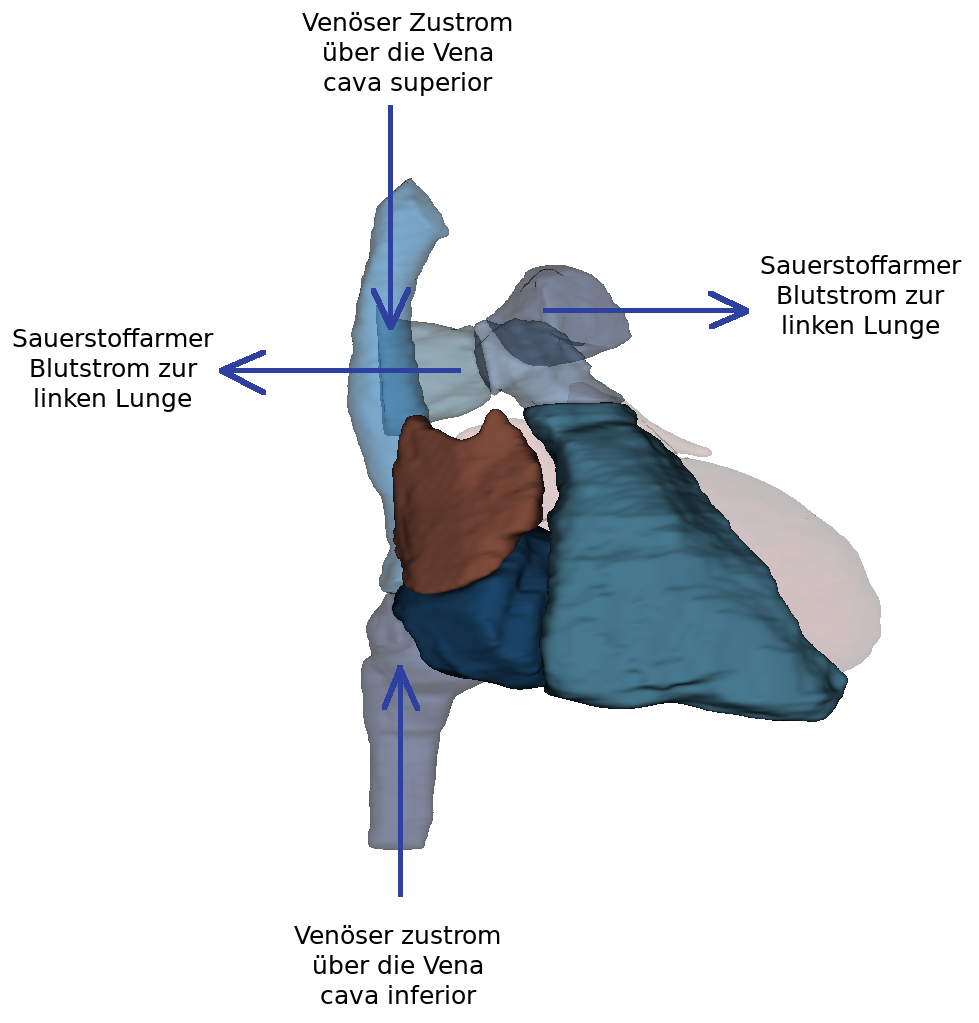
Inner spaces
In the heart, four internal spaces are distinguished (one chamber (ventricle) and one atrium (atrium) on the left and right respectively). The atria are adjacent to the ventricles, which are connected to the lungs or the major arteries and veins of the body by their outgoing vessels.
Inner spaces of the left heart
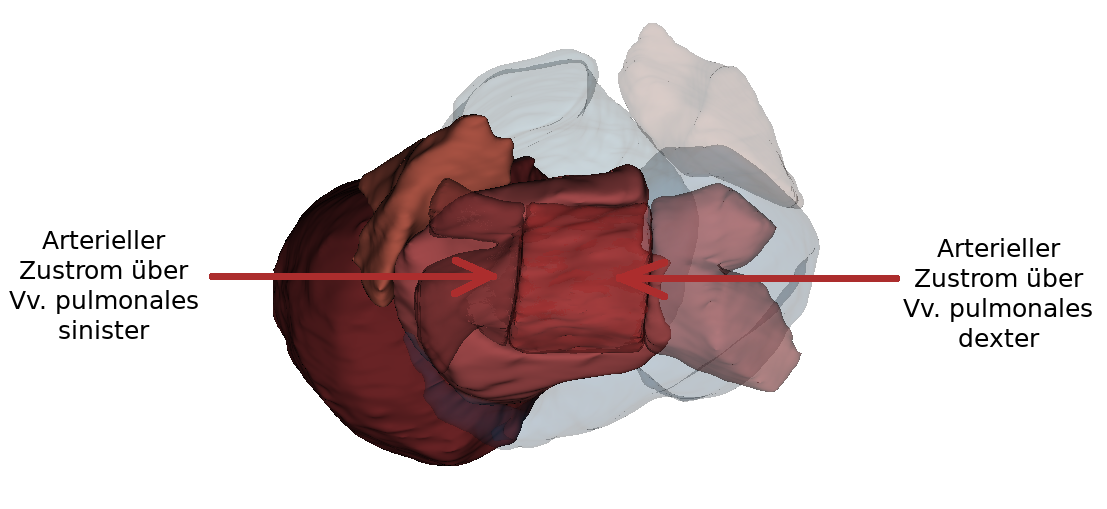
The left atrium has smooth walls between the openings of the four pulmonary veins (Vv. pulmonales dextra/sinistra superior and inferior). The muscle wall of the left atrium is thinner than that of the right atrium because it belongs to the low pressure system. The narrow fold (valvula foraminis ovalis) is temporarily visible at the septum interatriale. It is formed by raising the fossa ovalis into the left atrium.
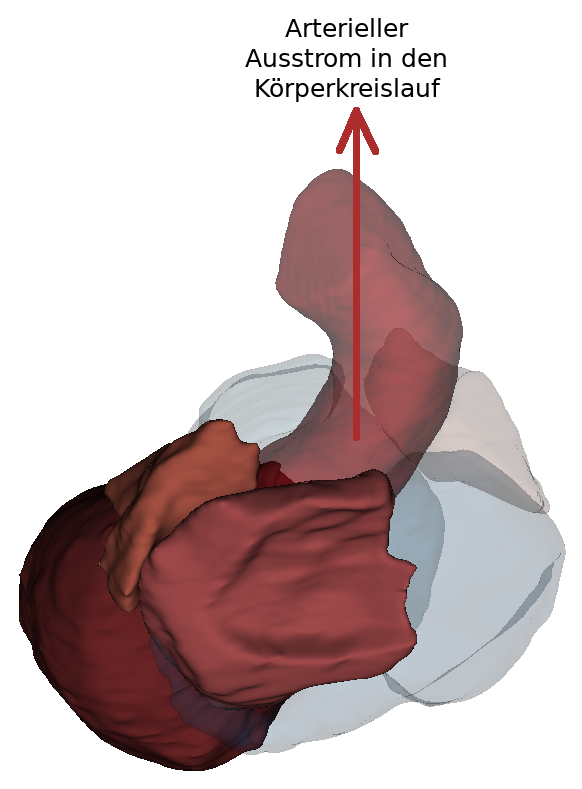
Blood passes from the left atrium into the left ventricle via the ostium atrioventriculare sinistrum.. The ostium atrioventriculare can be closed by the valva atrioventricularis sinistra. The left ventricle also has an inflow and outflow pathway. The inflow passes along the posterior wall, the left lateral wall as well as the apical section. The smooth-walled outflow tract is located near the septum interventriculare and continues into the vestibulum aortae. It consists largely of musculature (pars muscularis). The ostium aortae is the opening between the aortic outflow tract of the left ventricle and the aorta. The wall of the left ventricle is about three times as thick as that of the right ventricle and thus belongs to the high-pressure system.
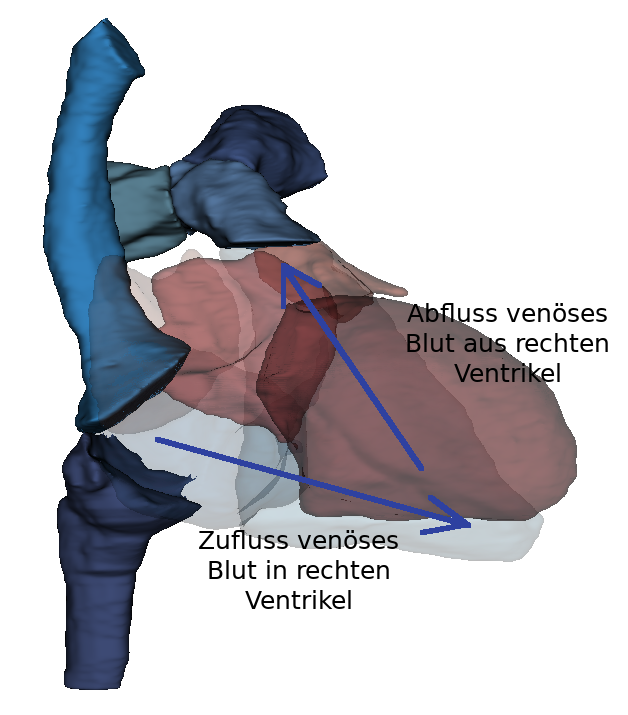
Inner spaces of the right heart
The posterior part of the right atrium consists of the sinus venarum cavarum (atrial sinus). At the ostium cavea superioris and inferioris the two vv. cavae (superior and inferior) open. From these, blood can flow seamlessly into the atrium without intervening valves. The oval fossa is located above the confluence of the inferior vena cava and is surrounded by the oval fossa limbus. The crista terminalis separates the anterior part (right atrium with heart ear) from the posterior.
The right atrium is larger than the left and also belongs to the low-pressure system. In contrast to the smooth-walled anterior section of the atrium, the posterior part has significantly more structure.
The right ventricle can also be separated into two parts by the trabeculae carnea and the crista supraventricularis.
The blood flows via the ostium atrioventriculare dextrum into the right ventricle. Here, too, there is an inflow and outflow trajectory. In the inflow area are the trabeculae carneae, which are small muscle bulbs. Here too, the papillary muscles are connected to the valva atrioventricularis (dextra) via chordae tendineae. The outflow tract continues over the conus arteriosus. The conus arteriosus is the cone-shaped transition of the right ventricle into the truncus pulmonalis. This area is smooth-walled and has no trabeculae carneae. The blood flows over the pulmonary valve (valva trunci pulmonalis) through the ostium trunci pulmonalis into the truncus pulmonalis. The right ventricle also belongs to the low-pressure system.
Overview of the heart valves
There are two types of valves in the heart: atrioventricular valves and vascular valves. The four heart valves serve to allow blood to flow in the heart in only one direction and thus prevent backflow of blood. The leaflet valves are located between the atria and the ventricles. The pocket valves are located between the pulmonary trunk and the aorta.
Sail valves (Valvae atrioventriculares)
The sail valves (valvae atrioventriculares) are also called atrioventricular valves (AV valves). They include the tricuspid valve (valva atrioventricularis dextra) and the bicuspid valve (valva atrioventricularis sinistra). These valves prevent the backflow of blood from the ventricles into the atria during contraction of the heart. The name of the valves comes from their shape, which resembles a sail. They project into the ostium atrioventricularis dextrum as well as sinistrum. The sail valves are attached to the musculi papillares via the chordae tendinae. These are a special form of the trabeculae carneae. Thus, the leaflet valves are mechanically attached to the cardiac skeleton.
During systole, the blood is forced out of the ventricle. In the process, the leaflet valves inflate and are filled with blood. The anchoring of the valves to the chordae tendinae and the contraction of the papillary muscles prevent the valves from opening into the atrium. The leaflet valves are located at the level of the ostium because the bulging of the leaflets towards the atrium is cancelled by the retraction of the papillary muscles.
Tricuspid valve
The tricuspid valve is located between the right atrium and ventricle. It prevents systolic backflow of blood from the right ventricle into the right atrium. It is made up of three leaflets: Cuspis anterior, cuspus posterior and cuspus septalis.
Bicuspid valve
The bicuspid valve is located between the left atrium and the left ventricle. Unlike the tricuspid valve, the bicuspid valve consists of only two leaflets (cuspis anterior and cuspis posterior).
Semilunar valves (Valvae semilunares)
The pulmonary valve and the aortic valve belong to the semilunar valves. Their structure is made up of a thin connective tissue with an endocardial covering. The valves are composed of three crescent-shaped pockets (valvula semilunaris anterior, sinistra and dextra) and open in the direction of the vessels in the ostium aortae or ostium trunci pulmonalis. The individual valves have a free edge (lunula valvae semilunares), which thickens in the middle to form a small connective tissue nodule (nodulus valvulae semilunaris). When the valve closes, the nodules and lunulae meet. In this way, the ostium is completely sealed. The backflow of blood is prevented by filling the pockets. No muscle contraction is necessary in this process.
Pulmonary valve (valva trunci pulmonalis)
The pulmonary valve prevents the backflow of blood into the right ventricle. Since this valve is located between two low-pressure systems (venous limb of the systemic circulation and pulmonary circulation), it is thinner.
Aortic valve (valva aortae)
The aortic valve prevents backflow from the aorta into the left ventricle. It has a slight outward bulge (sinus aortae). The coronary vessels ( a. coronaria sinistra and dextra) originate in the left and right sinus aortae, so that the heart is supplied with blood.
Cardiac auscultation
In the case of a malfunction, audible flow noises are caused by the formation of whirls in the blood. Cardiac auscultation is an old but important method for recognizing these sounds. It is used both for the initial detection and the follow-up of functional disorders. The basis is that two sounds can be heard in a healthy adult heart. The first heart sound (S1) is at the beginning of systole. The tone is produced by the blood column hitting the leaflet valves and not, as is often assumed, by the closure of the valves. The second heart sound (S2) is produced by the closure of the leaflet valves at the end of systole. It is much brighter than the first heart sound. The two sounds are clearly audible at different locations. The first heart sound is clearly heard above the apex of the heart, whereas the second heart sound is clearly heard above the base of the heart. At Erb's point, which is located on the left parasternal side in the third intercostal space, all heart valves can be detected equally well. Specific points on the chest are recommended for auscultation of individual heart valves, as the sounds are projected to these locations and can thus be heard loudest:
- Aortic valve: 2/3rd intercostal space right parasternal.
- Pulmonary valve: 2nd intercostal space left parasternal
- Tricuspid valve: 4th intercostal space right parasternal
- Bicuspid valve: 5th intercostal space left medioclavicular
Excitation formation and excitation conduction system (Coming soon)
In the heart there is an autonomous excitation generation system (systema conducente cordis) and an excitation conduction system (systema conducente cordis). A distinction is made between four sections. When the heart is excited, the atrial and ventricular muscles contract about 100,000 times a day. The heart muscle is controlled by electrical impulses. The resulting impulses spread through a special cell system of the heart muscle.
Sinus node
The sinus node is also called the nodus sinuatrialis or Keith-Flack node. Macroscopically, it consists of a muscular structure that is about 3 mm thick and 10 mm long. The external shape resembles a comma. It is located on the dorsal side of the right heart, subepicardially in the terminal sulcus. Cranial to the sinus node is the junction of the superior vena cava. In some cases, the sinus node extends into the right heart ear.
Functionally, the sinus node is the primary pacemaker centre of the heart and is therefore involved in the complex regulation of the heart rate. The sinus node has the central role of excitation formation. It generates excitation volleys with a resting frequency of 60-70 impulses per minute. The pulses are used to excite the atrial myocardium, as the atrial excitation wave propagates towards the ventricles. The sinuatrial ramus nodi provides blood flow to the sinus node. It is controlled by the sympathetic and parasympathetic nervous systems. The sinus node consists of specific heart muscle cells:
P cells
The P cells (pacemakers) are roundish, pale cells that are usually present in groups. They are connected to each other by nexus and desmosomes.
Transition cells
Transition cells are elongated and partially branched cardiomyocytes. They contain a large number of myofibrils. The transition cells connect the P cells and establish a connection to the working myocardium.
Atrioventricular node
The atrioventricular node is also called the nodus atrioventricularis, AV node or Aschoff-Tawara node. It is the secondary pacemaker centre of the heart. The AV node is 5 mm long, 3 mm wide and 1 mm thick and is located in the right atrium. Its exact location is at the base of the atrial septum before the confluence of the coronary sinus. This area is called the triangle of Koch. The atrioventricular node serves to regulate stimulus exaggeration via the non-conducting cardiac skeleton. It is continued by the His bundle, which continues towards the apex of the heart. The AV node is also controlled by the sympathetic and parasympathetic nervous systems. Blood flow takes place through the ramus nodi atrioventricularis from the arteria coronaria dextra. Its main function is to delay the transmission of excitation to the ventricles. This ensures that the atrial contraction is completed before the ventricular contraction begins. Spontaneous excitations can also be generated by the AV node. However, these have a much lower frequency (40-50 depolarisations per minute) than the sinus node. This impulse excitation does not take place as long as the sinus node is intact.
Atrioventricular bundle
The atrioventricular bundle, also known as the fasciculus atrioventricularis, AV bundle or His bundle, is a component of the heart's conduction system. It is 4 mm thick and 20 mm long. The AV bundle originates subendocardially in the atrium from the AV node. It penetrates the trigonum fibrosum dextrum and then divides into the two tawara legs in the pars membranacea of the ventricular septum. The function of the AV bundle is to transmit excitation from the AV node to the ventricular legs.
Bundle branch
The bundle branches are also called crus dextrum and sinistrum or tawara branches. The tawara legs divide at the AV bundle. Their main function is to transmit excitation from the His bundle via the nexus into the working myocardium. The left Tawara branch (crus sinistrum) branches off almost perpendicularly from the His bundle and then fans out. This creates the following structures: posterior fascicle, middle fascicle and anterior fascicle. The right tawara limb (crus dextrum) continues anteriorly and enters the myocardium of the ventricular septum. It continues towards the apex of the heart. In the ventricular myocardium, excitation is transmitted via the Purkinje fibres.
Diseases
Free exploration
- Heart
- Heart vessels
- Internal spaces in the heart
- Heart in situ
Look at the heart in 3D and explore it freely. Afterwards, you can look at other cases or check your acquired knowledge through the practice exercises.
Look at the vessels that connect the heart to the body and pulmonary circulation as well as some coronary vessels.
Look at the internal spaces in the individual parts of the heart.
Look at the heart in situ.